Osteochondral Lesion Talus Surgery
An osteochondral lesion of the talus (OLT or OCD) is a cyst, tear, or fracture in the cartilage of the talus. The talus is a bone located between the tibia and fibula, forming part of the lower ankle joint. The majority of these lesions are associated with sports injuries and trauma; in particular, they are ankle sprains or fractures, but there are also non-traumatic osteochondral talus lesions (osteochondritis dissecans) that can cause similar ankle pain and dysfunction.
OLT/OCD’s can be difficult to diagnose as ankle pain, and the most common symptom is non-specific. You may have experienced an ankle sprain that never recovers, with swelling, clicking, locking, cathing, and popping on movement. First-line management is non-surgical treatment for the OLT/OCD that includes rest, ankle immobilization in a boot or brace, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs). If these treatments fail, surgery becomes necessary.
What Is Osteochondral Lesion of the Talus Surgery?
Osteochondral lesion of the talus, or OLT/OCD, surgery is orthopedic surgery that is undertaken to repair cartilage damage to the talus. Depending on the size of the cartilage lesion, your surgeon can drill the underlying bone to promote healing (microfracture surgery), graft healthy cartilage from a non-weight-bearing part of the ankle or knee, or use biologics to graft to the lesion.
What Are the Goals of Osteochondral Lesion of the Talus Surgery?
OLT/OCD surgery helps to restore a normal articular surface by inducing the development of repair tissue that can heal properly, perform similarly to normal cartilage, and promote normal joint function. Other objectives of surgery include the following:
- Pain relief
- Stabilization of the ankle joint
- Removal of loose cartilage
- Resumption of a normal level of mobility
- Reduction of the risk of osteoarthritis
What Does Osteochondral Lesion of the Talus Surgery Involve?
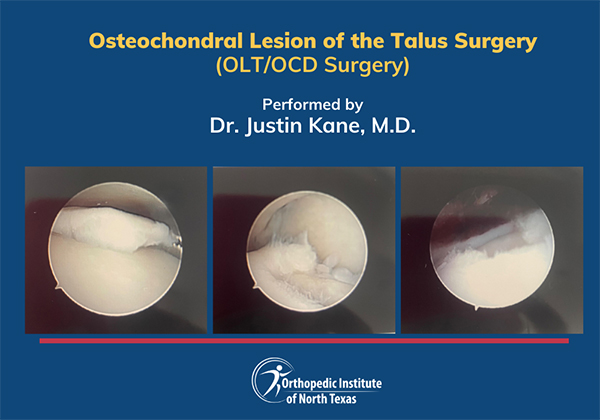
OLT/OCD surgery uses arthroscopy – a keyhole surgery that is ideally suited to safely access the interior surfaces of the ankle joint. This type of minimal-access surgery uses an arthroscope, a long narrow tube that is lined with optical fiber and attached to a camera. Your surgeon uses this camera to view the operative site during the treatment of the osteochondral lesion of the talus.
The precise nature of the surgery depends on the size and location of the OLT/OCD, as well as the overall stability of the joint. Large lesions or extensive joint instability may mean that your surgeon may need to perform an alternate operation called Osteochondral Autologous Transfer Surgery (OATS).
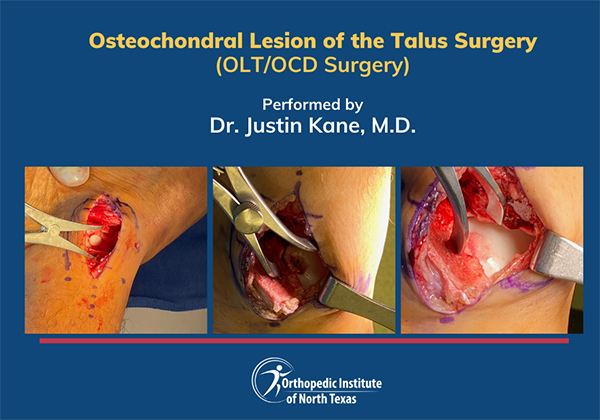
Your surgeon will operate via two small incisions at the front of your ankle. Through these incisions, thin surgical instruments are used to remove any loose cartilage, cyst, or bone fragments. Lesions are then drilled to the bone marrow layer to stimulate bleeding, which covers the lesion and promotes the development of a new cartilage layer.
Larger osteochondral lesions require more complex intraoperative management. Arthroscopy and drilling are less likely to be successful where lesions are larger than 150mm2. Instead, Osteochondral Autologous Transfer Surgery (OATS) is used to graft cartilage plugs taken from non-weight-bearing parts of the ankle joint or knee in the lesion. This procedure is most suitable where more significant cartilage defects are isolated.
What Factors Affect OLT/OCD Talus Surgery Success?
OLT/OCD surgery success is primarily determined by the size of the cartilage lesion. Studies and clinical reviews indicate that arthroscopy and drilling of smaller lesions have the best outcomes, with a 75% success rate where lesions are less than 150 mm².
Who Is a Suitable Candidate for OLT/OCD Surgery?
The patients who benefit most from OLT/OCD surgery usually have chronic lesions with displaced cartilage, where conservative management has failed to improve pain and mobility. Early surgery can also benefit some patients, such as those with displaced cartilage floating in the joint or acute osteochondral talus fractures with displacement or cystic subchondral lesions covered by intact cartilage that benefit from drilling to induce bone healing.
What Does Postoperative Recovery From OLT/OCD Surgery Involve?
OLT/OCD surgery is routinely performed as a day surgery. Once the arthroscopy is completed, the foot is dressed with bandages that should not be disturbed until your surgeon reviews you at your first follow-up appointment and removes your stitches. Keep your foot elevated as much as possible. We'll provide anti-inflammatory medication to reduce swelling and pain and crutches to keep you mobile.
Expect to rest for the first two weeks post-operatively, but at your surgeon's direction, you can begin to walk, drive, and return to work activities. At six weeks, most patients can resume a majority of their previous level of daily activity. Care must be taken to avoid twisting or impacting the ankle for at least two to three months and a return to sports should only be attempted after consultation with your surgeon.
Justin M. Kane, M.D.
Board Certified Foot & Ankle Orthopedic Surgeon
Justin M. Kane, MD, is an orthopedic surgeon educated at Rensselaer Polytechnic and Thomas Jefferson University. He trained at Temple University Hospital and completed his residency at The Rothman Institute at Thomas Jefferson University Hospital. Following a foot and ankle surgery fellowship at Baylor University Medical Center, he practiced at Baylor and directed research at the Human Motion and Performance Center.
Dr. Kane founded the Orthopedic Institute of North Texas, where he treats a range of foot and ankle conditions and performs advanced reconstructive surgeries. He has published extensively and contributes to orthopedic education and research.
Beyond his practice, Dr. Kane is involved in international medical missions, including in Vietnam with AOFAS and MOI, and in the Dominican Republic with Rush University. His personal interests include cycling, golf, international cooking, and animal rights activism.
Considering OLT/OCD Surgery? Talk to Dr. Kane
Osteochondral lesions of the talus are a challenging orthopedic condition that requires thorough investigation and attentive care. Our skilled and experienced multi-disciplinary team and foot and ankle fellowship-trained orthopedic surgeons at the Orthopedic Institute of North Texas are on hand to help you navigate OLT/OCD care and maximize your mobility. Contact Dr. Kane today to schedule a consultation to explore your treatment options.
Frequently Asked Questions
What Does the Preoperative Protocol for OLT/OCD Surgery Involve?
Our surgeons use a combination of radiographs, computed tomography (CT), and high-resolution magnetic resonance imaging (MRI) to assess the damage to the cartilage in order to determine treatment options. An anesthetia team will provide a comprehensive anesthetic assessment to establish your fitness for surgery.
What Are the Risks and Complications of OLT/OCD Surgery?
The main risk of OLT/OCD surgery is ongoing stiffness, pain, and recurrent problems with your ankle that require a repeat arthroscopy or more extensive surgery. Other risks of this operation include nerve injury with altered sensation across the top of the foot and scar sensitivity that can be reduced by massage.
